Heart rate measurement:
Heart rate is the number of heartbeats per unit of time. Usually heart rate is expressed as beats per minute (BPM). The heart beats to supply oxygenated clean blood from the left ventricle to the blood vessels of the body via the aorta. As the need for oxygen changes in various situations, like exercise, sleep and so forth, the heart rate changes accordingly. Normally humans have their heart rate between 70 to 90 beats per minute.
How is heart rate measured?
Heart rate is usually measured by finding the pulse in the body. The pulse is felt by the pads of the index and middle fingers of the examiner.
At each beat, the heart pumps blood into the blood vessels. As the blood flows into the blood vessels the blood vessels expand and this is felt as a pulse.
This pulse rate is felt at any part of the body where the arterial pulsation is transmitted to the skin surface especially when it is compressed against an underlying structure like bone.
Some of the pulse sites include:-
• Temporal artery by the sides of the forehead
• Facial artery at the angle of the jaws
• Carotid artery in the neck
• Brachial artery
• Radial artery at the wrist
• Dorsalis pedis artery over the foot
Other ways to measure the heart rate
Pulse rate or heart rate can also be determined by using an electrocardiograph, or ECG or heart rate monitors. Heart rate monitors allow accurate measurements of the heart rate during exercise as well as during rest.
Respiration rate Measurement:
The respiration rate is the number of breaths a person takes per minute. The rate is usually measured when a person is at rest and simply involves counting the number of breaths for one minute by counting how many times the chest rises. Respiration rates may increase with fever, illness, and other medical conditions. When checking respiration, it is important to also note whether a person has any difficulty breathing.
Normal respiration rates for an adult person at rest range from 12 to 16 breaths per minute.
Blood pressure Measurement:
Blood pressure is the force of the blood pushing against the artery walls during contraction and relaxation of the heart. Each time the heart beats, it pumps blood into the arteries, resulting in the highest blood pressure as the heart contracts. When the heart relaxes, the blood pressure falls.
Two numbers are recorded when measuring blood pressure.
The higher number, or systolic pressure, refers to the pressure inside the artery when the heart contracts and pumps blood through the body.
The lower number, or diastolic pressure, refers to the pressure inside the artery when the heart is at rest and is filling with blood.
Both the systolic and diastolic pressures are recorded as "mm Hg" (millimeters of mercury). This recording represents how high the mercury column in an old-fashioned manual blood pressure device (called a mercury manometer or sphygmomanometer) is raised by the pressure of the blood.
High blood pressure, or hypertension, directly increases the risk of heart attack, heart failure, and stroke. With high blood pressure, the arteries may have an increased resistance against the flow of blood, causing the heart to pump harder to circulate the blood.
Blood pressure is categorized as normal, elevated, or stage 1 or stage 2 high blood pressure:
• Normal blood pressure is systolic of less than 120 and diastolic of less than 80 (120/80)
• Elevated blood pressure is systolic of 120 to 129 and diastolic less than 80
• Stage 1 high blood pressure is systolic is 130 to 139 or diastolic between 80 to 89
• Stage 2 high blood pressure is when systolic is 140 or higher or the diastolic is 90 or higher
These numbers should be used as a guide only.
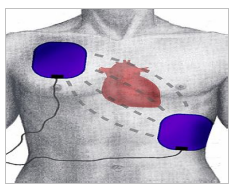
Defibrillator Working Principle:
A defibrillator delivers a dose of electric current (often called a counter-shock) to the heart. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm.
Defibrillators can be external, transvenous, or implanted depending on the type of device used or needed.
A method to return the heart muscle fibers to its normal synchronized working is called defibrillation. It consists of delivering a dose of electric energy to the affected heart with a device called defibrillator.
Depending on this fibrillation is classified into atrial fibrillation of atrial muscles and the fibrillation of ventricles is called ventricular fibrillation.
The early defibrillators used the alternating current which is transformed from normal line voltage up to 300-1000 volts from a power socket to the exposed heart by way of paddle type electrodes. This application of an electrical shock to resynchronize, the heart is called counter shock. If the patient does not respond, the method is repeated until defibrillation occurs. This method of defibrillation is called AC defibrillation. Nowadays this type of defibrillation is not used because it has some disadvantages. This technique was often unsuccessful and showed harm to the cells of heart muscle post mortem. So DC defibrillators are commonly used now.
DC DEFIBRILLATORS:
A scientist named Bernard Lown used an alternating method which involved the charging of bank capacitors to approximately 1000 Volts and then delivering the charge through an inductance such as to produce a heavily damped sinusoidal wave of finite duration. So in DC defibrillation method, a capacitor is charged to a high dc voltage and is then allowed to discharge rapidly. The defibrillator is designed in such a way that the capacitor is rapidly discharged through electrodes across the chest of the patient.
Principle of Pacemaker:
A pacemaker is a small device that's placed (implanted) in the chest to help control the heartbeat. It's used to prevent the heart from beating too slowly. Implanting a pacemaker in the chest requires a surgical procedure. Pacemakers work only when needed. If your heartbeat is too slow (bradycardia), the pacemaker sends electrical signals to your heart to correct the beat.
A pacemaker has two parts:
• Pulse generator. This small metal container houses a battery and the electrical circuitry that controls the rate of electrical pulses sent to the heart.
• Leads (electrodes). One to three flexible, insulated wires are each placed in one or more chambers of the heart and deliver the electrical pulses to adjust the heart rate. However, some newer pacemakers don't require leads. These devices, called leadless pacemakers, are implanted directly into the heart muscle.
What is Medical Electronics Equipment ?
Medical Electronics engineers are the one who design devices that solve medical and health-related problems by combining their knowledge of biology and medicine with engineering principles and practices. Medical Electronics engineers also design devices used in various medical procedures, imaging systems such as magnetic resonance imaging (MRI), and devices for automating insulin injections or controlling body functions. Medical electronic devices include pacemakers, drug-releasing pumps, hearing aids, and diagnostic equipment for measuring, monitoring, and recording body functions such as heartbeat and brain waves.
Classification of Diagnostic Laboratory Equipment:
Diagnostic equipment includes medical imaging machines, used to aid in diagnosis. Examples are Ultrasound and MRI machines, CT scanner and x-ray machines. Ultrasound or ultrasonography is a medical imaging technique that uses high frequency sound waves and their echoes. The technique is similar to the echolocation used by bats, whales and dolphins, as well as SONAR used by submarines. In ultrasound, the following events happen:
1. The ultrasound machine transmits high-frequency (1 to 5 megahertz) sound pulses into your body using a probe.
2. The sound waves travel into your body and hit a boundary between tissues (e.g. between fluid and soft tissue, soft tissue and bone).
3. Some of the sound waves get reflected back to the probe, while some travel on further until they reach another boundary and get reflected.
4. The reflected waves are picked up by the probe and relayed to the machine.
5. The machine calculates the distance from the probe to the tissue or organ (boundaries) using the speed of sound in tissue (1,540 m/s) and the time of the each echo's return (usually on the order of millionths of a second).
6. The machine displays the distances and intensities of the echoes on the screen, forming a two dimensional image like the one shown below.
MRI:
Classification of Therapeutic Laboratory Equipment:
Classification of Clinical Laboratory Equipment:
Bioelectric signals:
Bioelectrical signals are very low amplitude and low frequency electrical signals. These signals can be measured from biological beings, for example, humans. Bioelectrical signals are generated from the complex self-regulatory system and can be measured through changes in electrical potential across a cell or an organ. Their basic source is the cell membrane potential which under certain conditions may be excited to generate an action potential. The electric field generated by the action of many cells constitutes the bio-electric signal. The most common examples of bioelectric signals are the ECG (electro cardio graphic) and EEG (electro encephalo graphic) signals.
Bioacoustic
Signals: The examples of such signals are: flow of blood in the heart, through the heart’s valves and flow of air through the upper and lower airways and in the lungs which generate typical acoustic signal.
Biomechanical Signals:
The movement of the chest wall in accordance with the respiratory activity is an example of this type of signal.
Biochemical Signals:
The signals which are obtained as a result of chemical measurements.
Biomagnetic
Signals: Extremely weak magnetic fields are produced by various organs such as the brain, heart and lungs.
Bio-impedance Signals:
The measurement of galvanic skin resistance is a typical example of this type of signal.
Bio Electrodes: Bioelectrodes can be classified as:
• Surface electrodes: These electrodes pick up potentials from the surface of the tissue.
• Deep seated electrodes: These electrodes are inserted inside a live tissue or cell.
The materials used to make Electrodes include:
• Aluminium (Al)
• Copper (Cu)
• Silver (Ag)
• Gold (Au)
• Platinum (Pt)
The three basic types of biopotential electrodes used in biomedical measurements are:
1. Microelectrodes
2. Skin surface electrodes
3. Needle electrodes
These electrodes are designed to measure bioelectric potentials near or within the cell.
(1) Microelectrodes can be of two types:
• Metal
• Micropipette
Metal microelectrodes are formed from a fine needle of a suitable metal down to a fine tip. Then the needle is coated almost to the tip with an insulating material.
Skin Surface Electrodes
.png)
Needle Electrodes:
An electro cardio gram (ECG) is one of the simplest and fastest tests used to evaluate the heart. Electrodes (small, plastic patches that stick to the skin) are placed at certain spots on the chest, arms, and legs. The electrodes are connected to an ECG machine by lead wires. The electrical activity of the heart is then measured, interpreted, and printed out. No electricity is sent into the body.
A typical flexible biopotential electrode for ECG (electrocardiogram, ECG) recording is composed of certain polymers or elastomers which are made electrically conductive by the addition of a fine carbon or metal powder. The most common type of biopotential electrode is the silver/silver chloride electrode (Ag/AgCl), which is formed by electrochemically depositing a very thin layer silver chloride onto the surface of silver electrode. These electrodes are recessed and imbedded in foam that has been soaked with an electrolyte paste to provide good electrical contact with the skin. The electrolyte saturated foam is also known to reduce motion artifacts which are produced during stress testing when the layer of the skin moves relative to the surface of the Ag/AgCl electrode. This motion leads to the large interference in the recorded biopotential and, in the extreme cases, could severely degrade the measurement.
ECG Machine Block Diagram:
1. Electrodes:
2. Lead selector:
3. Pre-amplifier:
4. Driver:
5. PMMC Galvanometer:
6. Hot - tip stylus and stylus heater:
7. Recorders:
Applications:
EEG
EEG Machine Block Diagram:
1. Montage selector:
2. Pre-amplifier
3. Filters and amplifiers
4. Analog to Digital Converters (ADC)
5. Writing recorder and paper drive
THANKS FOR READING







.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
0 Comments